Information about breast cancer
Risk factors for breast cancer
- No specific causative factors are known, but some relative risk factors are identified.
- Increasing age, but age is no bar.
- Sex - more common in females. Though uncommon in men, is known to occur.
- Family history of breast cancer in first degre relative - mother, sister, daughter, maternal aunt maternal grandmother.
- Genetic factor- if brca1 and brca2 are positive [mutations in brca 1 and brca2 genes] 70-80% chances of getting breast cancer during lifetime [genetic study for brca1 and brca2 genes is done in specialised centres]
- H/o breast cancer in opposite breast
- Hormonal factors
- - Long term use of oral contraceptive pills (more than 10 years]
- - Early menarche(before 11 yrs.)
- - Late menopause (beyond 55-60 yrs)
- - Late first child (after 30 yrs.)
- - Nulliparous, unmarried females or not breast fed their babies for 1 year
- - Hormone replacement therapy - HRT for many years.
- Consumption of fatty food- containing animal fat and saturated fat - obesity
- History of radiation to upper body parts - delayed presentation.
How can early diagnosis be done
- Regular clinical examination [checkup from doctor] , even if no symptoms, once a year
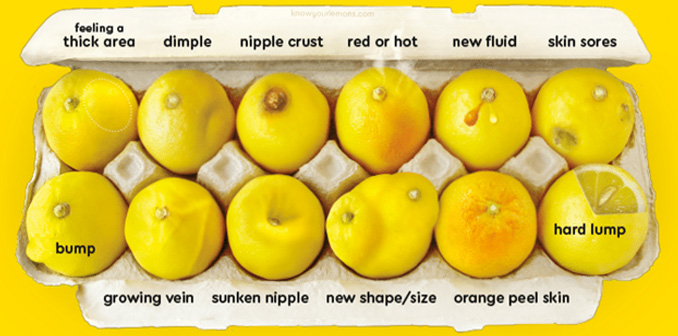
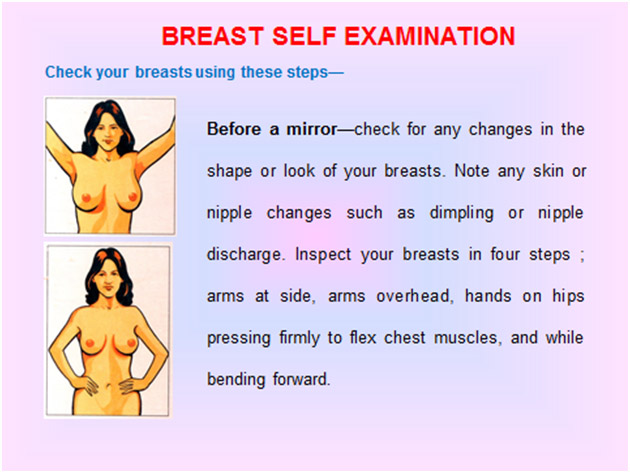
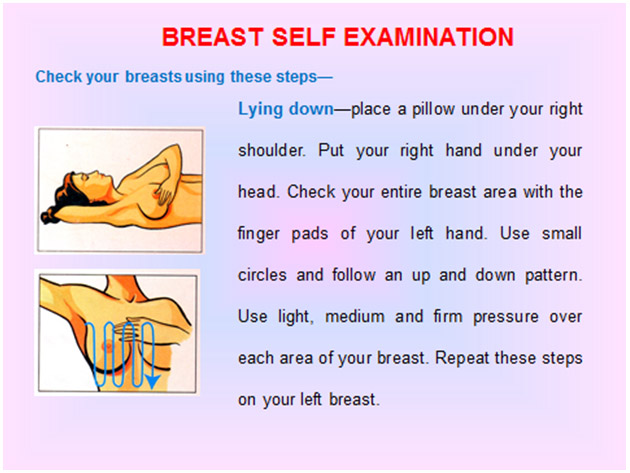
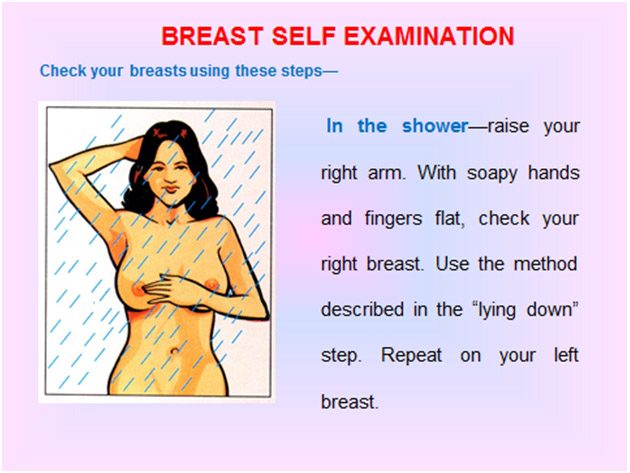
- Self breast examination once a month ,[ 5-6 days after period is over] , any one predecided day of the month for postmenopausal women
- Mammography every 2 years after the age of 40 and every year after the age of 50
- MRI in high risk group patients
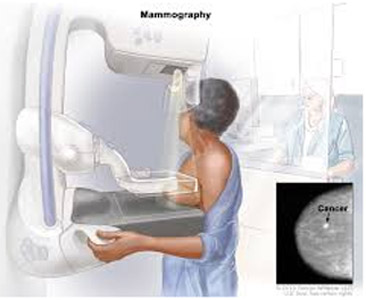
About mammography
- A mammogram is a special x-ray of breast
- Mammograms can reveal 90% growths, both harmless and cancerous - upto 1 to 2 years before they can be felt by hand.
- Hence can detect cancer/growth when it is quite small [in very early stage] and so can be completely cured.
- Two yearly after the age of 40, yearly after the age of 50
- High risk patients and patients with family history of breast cancer should get mammography done as and when advised by doctor

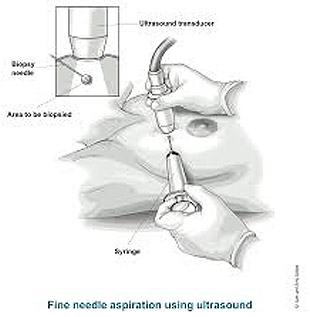
FNAC [fine needle aspiration cytology]
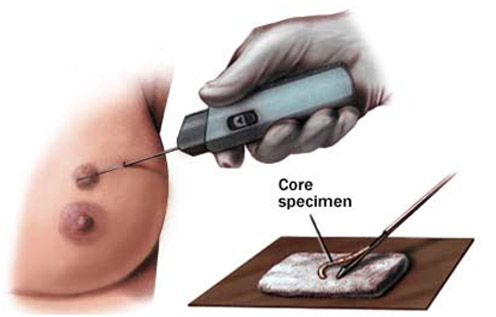
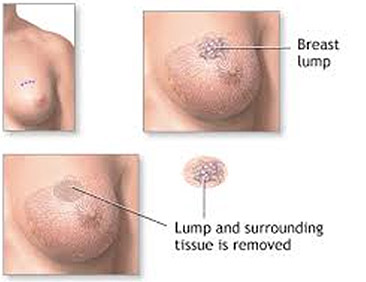
Core Biopsy & Excisional Biopsy
Treatment of breast cancer
Treatment of breast cancer depends upon following factors
- Stage of cancer
- Size of lump
- General condition of the patient
- Patient's wish
- Patient is premenopausal / postmenopausal
1) Surgery
a) Breast conservation surgery
- If diagnosed in early stage and lump small in size, breast can be conserved [ saved ]. Hence the importance of early detection.
- Wide excision of lump with clear margins [taking out the lump keeping some normal tissue around ]
- Total axillary clearance [ excising all lymph nodes in armpit.]
- Post surgery radiotherapy is mandatory with breast conservation.
b) Mastectomy
- Removal of entire breast including the nipple and areola.
- Removal of lymph nodes in the axilla [armpit ]
2) Chemotherapy
- Chemotherapy are injections given intravenous [ in veins ]
- Chemotherapy is given if -
- If the cancer has spread beyond the breast - to the lymph nodes in armpit or other parts of the body
- Tumor > 2cm
- Premenopausal high risk patients
- Depends on hormone receptor status of the tumor
3) Radiotherapy
- Radiotherapy is giving radiation [ targeted x-ray ] to the breast in view of destroying cancer cells.
- Radiotherapy is given if -
- - After surgery, in case of large tumors and if skin is involved.
- - If cancer has spread to other parts of body.
- - If cancer has spread to more number of axillary lymph nodes
- - In all patients undergoing breast consevation surgery
4) Hormonal Therapy
- Hormone therapy [ oral tablets ] contains antiestrogen drug .
- It is given in patients having estrogen and progesterone receptor positive tumors
- Decreases / prevents disease recurrence in hormone receptor positive patients.
- To be taken for 5 to 10 years
5) Immunotherapy
- Immune modulators are given as adjuvant therapy.
- Given in patients with tumors that has a protein receptor called her 2
Recent Advances
Immunotherapy facts & Hopes - Breast cancer poses threat to health & wellness of women. Surgery, chemotherapy, radiotherapy are standared treatments. Over past few years hormone receptors ER, PR & HER 2 testing has become routine & treatment as per the ER, PR HER to status has become the standard of care. Immunotherapy is used in many solid tumors. Immune system plays a role in breast tumor growth & its progression & elimination. Some triple negative breast cancers are aggressive and difficult to treat. TNBC are more likely to express(PDL1) Programmes Death Ligend one. They can be benefited by immunotherapy eg. CTLA-4 blockage , Ipilumunab, Pemprolizumab, Avelumab, Atezolizumab. Breast cancers vaccines are designed to induce or amplify tumor specific T cells which can detect & destroy tumors cells.
More about hormone therapy and immunotherapy
- For deciding this mode of therapy, certain bio markers are evaluated and looked for in the tumor tissue
- Evaluation of presence of hormone receptors [estrogen receptors and progesterone receptors, ER and PR]
- Evaluation of excess levels of Human Epidermal growth receptor 2 [HER 2].
- If the Breast cancer is ER,PR +ve and HER 2 -ve, then the prognosis is better than ER PR +ve and HER 2 +ve
- For triple negative breast cancers [i.e. ER -ve, PR -ve and HER 2 -ve] the prognosis is relatively poor.
- For ER PR +ve cancers, endocrine {hormone } therapy is given which works by blocking the effects of the hormone estrogen or lowering its level.
-
Currently available drugs include -
- Tamoxifen [ antiestrogen] It blocks the uptake of estrogen by the ER
- aromatase inhibitors [ letrozole and anastozole] which suppress the conversion of androgens to estrogen thus resulting in estrogen depletion.
- LHRH analogs. [Goserelin] which suppress the estrogen secretion by ovaries
- For HER 2 +ve cancers
- Herceptin [Trastuzumab] a monoclonal antibody is given ,alone or in combination of other chemotherapy.
6) Newer advances in breast cancer surgery
- Skin sparing mastectomy - where the skin is preserved as much as possible , so breast reconstruction is possible immediately and gives a better cosmetic result.
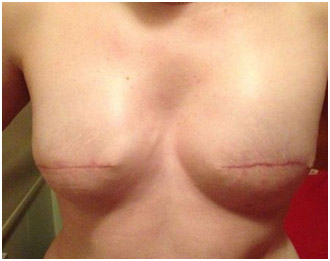
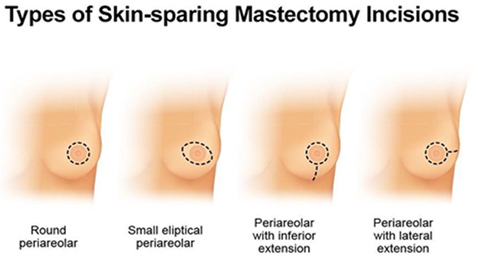
- Oncoplastic surgery - where incisions are placed in such a way that cosmetic outcome is good and lumps can be removed by hiding the incisions as much as possible.
7) Follow up of patients treated for breast cancer
- Regular follw up with your treating doctor.
- Physical examination every 3-6 months for first 3 years and every 6-12 months for next 2 years i.e. upto 5 years.
- After 5 years, yearly check up.
- Mammography (MMG)every year of opposite breast for those who have undergone mastectomy.
- Those who have undergone breast conserving surgery, a post treatment MMG should be done 1 year after the initial MMG and 6 months after completion of radiotherapy.
- Monthly self breast exam of opposite breast
- Regular gynaec check ups, particularly for pts. taking Tamoxifen. Should report immediately if vaginal bleeding or spotting after menopause or any abnormal bleeding or spotting between periods or change in periods.
- Look for any local recurrence of lump
- If recurrence, the treating doctor will decide regarding the appropriate treatment depending on the situation( surgery and radiotherapy or chemotherapy).
- According to symptoms, ultrasound of liver, chest X ray and MRI/CT may be required to do.